It’s been an exciting month for patient safety in the region’s Mental Health community.

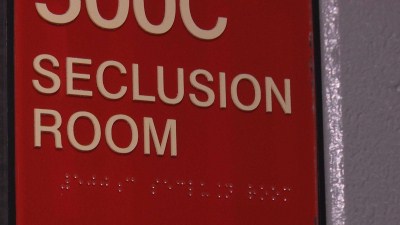
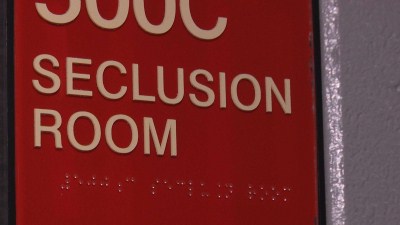
 The first event facilitated by AHSN Improvement Academy (using the hashtag #iaseclusion) brought together clinicians, managers, policy makers (Department of Health) and the quality regulator (CQC) from across Yorkshire and Humber to focus on reducing the use of seclusion, and where it has to be used, to make it safer and less traumatic. Seclusion and forced medication are major concerns for staff, users and policy makers alike; understanding the reasons behind coercive interventions is a crucial step in reducing their use and making care safer for both service users and staff. The University of Leeds’ School of Healthcare is involved in a number of projects in this area including; a PhD examining seclusion practices in the North East, and involvement in a major quality improvement programme in the North West in which six key core strategies are implemented to reduce the harm associated with restraint (funded by the Health Foundation ) and a collaboration between universities, NHS Trusts and the Advancing Quality Alliance/AQUA .
The first event facilitated by AHSN Improvement Academy (using the hashtag #iaseclusion) brought together clinicians, managers, policy makers (Department of Health) and the quality regulator (CQC) from across Yorkshire and Humber to focus on reducing the use of seclusion, and where it has to be used, to make it safer and less traumatic. Seclusion and forced medication are major concerns for staff, users and policy makers alike; understanding the reasons behind coercive interventions is a crucial step in reducing their use and making care safer for both service users and staff. The University of Leeds’ School of Healthcare is involved in a number of projects in this area including; a PhD examining seclusion practices in the North East, and involvement in a major quality improvement programme in the North West in which six key core strategies are implemented to reduce the harm associated with restraint (funded by the Health Foundation ) and a collaboration between universities, NHS Trusts and the Advancing Quality Alliance/AQUA .
 In Leeds, NIHR CLAHRC Yorkshire and HumberResearch Capacity funding has allowed us to begin work examining mechanisms to reduce polypharmacy of psychotropic medications. Polypharmacy – multiple prescriptions of the same type of drug – reduces life expectancy and has side effects that make care less safe; particularly when more than one antipsychotic medication is being prescribed. Repeated national attempts led by the Prescribing Observatory for Mental Health (POMH) to influence prescribing habits via clinical audit and feeding back the results to Trusts have had only modest success. We think that service user involvement in designing interventions to change professional behaviour is an under explored dimension of the strategies used so far to tackle this “sticky” healthcare issue. Medication is a complicated element of the relationship between service users and the professionals that support them. Before asking service users about what makes involvement in these kinds of choices difficult or easier, we are going to systematically examine the literature on others’ attempts to share the development of interventions with service users. A nurse from Leeds & York NHS Partnership Trust has been seconded to help us work on this project and improve the chances of any intervention being feasible in the “real world” of clinical practice.
In Leeds, NIHR CLAHRC Yorkshire and HumberResearch Capacity funding has allowed us to begin work examining mechanisms to reduce polypharmacy of psychotropic medications. Polypharmacy – multiple prescriptions of the same type of drug – reduces life expectancy and has side effects that make care less safe; particularly when more than one antipsychotic medication is being prescribed. Repeated national attempts led by the Prescribing Observatory for Mental Health (POMH) to influence prescribing habits via clinical audit and feeding back the results to Trusts have had only modest success. We think that service user involvement in designing interventions to change professional behaviour is an under explored dimension of the strategies used so far to tackle this “sticky” healthcare issue. Medication is a complicated element of the relationship between service users and the professionals that support them. Before asking service users about what makes involvement in these kinds of choices difficult or easier, we are going to systematically examine the literature on others’ attempts to share the development of interventions with service users. A nurse from Leeds & York NHS Partnership Trust has been seconded to help us work on this project and improve the chances of any intervention being feasible in the “real world” of clinical practice.

 The focus on mental health and patient safety in the AHSN has provided a great opportunity to bring together some of the best in applied health research in the region, as well as those in the NHS who are keen to see evidence based innovation implemented and evaluated to improve services. Two CLAHRC Themes are represented in the work (Mental Health and Co-Morbidities and Evidence-Based Transformation in the NHS) as well as staff from the Mental Health providers in the Region in the Patient Safety Collaborative Network. This kind of “joined-up” partnership working to address problems that are resistant to just the NHS, or just academia. Tackling is exactly the kind of thing that the improvement academy was established to address. Safety is rarely a “sexy” topic in healthcare but we hope that the collaboration between the CLAHRC and the AHSN’s Improvement Academy – bringing together innovation, research evidence, and the best in patient centred NHS improvement – goes some way towards making mental healthcare in the region safer.
The focus on mental health and patient safety in the AHSN has provided a great opportunity to bring together some of the best in applied health research in the region, as well as those in the NHS who are keen to see evidence based innovation implemented and evaluated to improve services. Two CLAHRC Themes are represented in the work (Mental Health and Co-Morbidities and Evidence-Based Transformation in the NHS) as well as staff from the Mental Health providers in the Region in the Patient Safety Collaborative Network. This kind of “joined-up” partnership working to address problems that are resistant to just the NHS, or just academia. Tackling is exactly the kind of thing that the improvement academy was established to address. Safety is rarely a “sexy” topic in healthcare but we hope that the collaboration between the CLAHRC and the AHSN’s Improvement Academy – bringing together innovation, research evidence, and the best in patient centred NHS improvement – goes some way towards making mental healthcare in the region safer.